Depression: breakthroughs in Individual Therapy
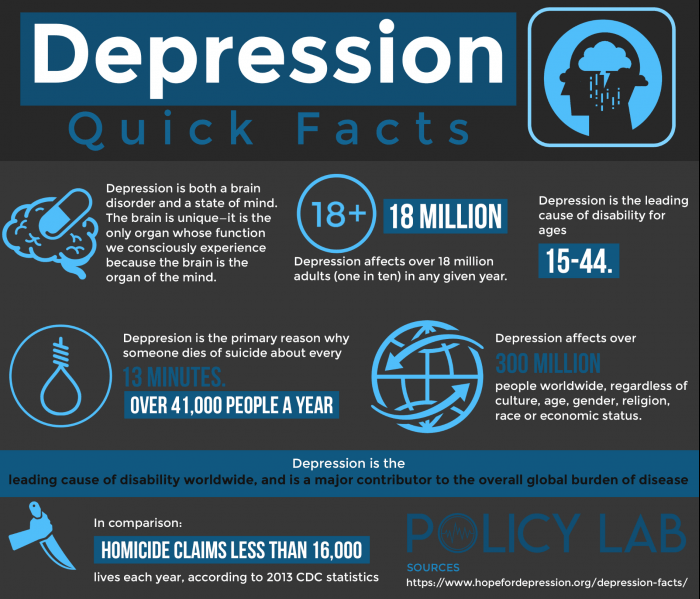
- A major depressive disorder is a serious medical illness affecting an estimated 18 million American adults.
- CDC estimates that 8.1 percent of American adults ages 20 and over had depression in any given 2-week period from 2013 to 2016.
- One in eight middle-aged women in the United States has depression, a new report finds.
- This means that women ages 40 to 59 have the highest rate of depression (12.3 percent) of any group based on age and gender in the U.S., according to the report from the Centers for Disease Control and Prevention.
- Among Americans ages 12 and older, 9.5 percent of females and 5.6 percent of males had moderate or severe depression
- Abuse. Past physical, sexual, or emotional abuse can cause depression later in life.
- The focus of Individual Therapy efforts center on areas of individuals’ lives that they have a concern. These areas commonly involve conditions that are causing a great deal of distress in the individual’s life. Individual therapy has proven fundamental in treating depression.
WHAT IS DEPRESSION?
Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think and how you act. Fortunately, it is also treatable. Depression causes feelings of sadness and/or a loss of interest in activities once enjoyed. It can lead to a variety of emotional and physical problems and can decrease a person’s ability to function at work and at home.
Depression is a common but serious mood disorder. It causes severe symptoms that affect how you feel, thinks and handle daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least two weeks.
Some forms of depression are slightly different, or they may develop under unique circumstances, such as:
• Persistent depressive disorder
• Postpartum depression
• Psychotic depression
• Seasonal affective disorder
• Bipolar disorder high – euphoric or irritable – moods called “mania” or a less severe form called “hypomania.”
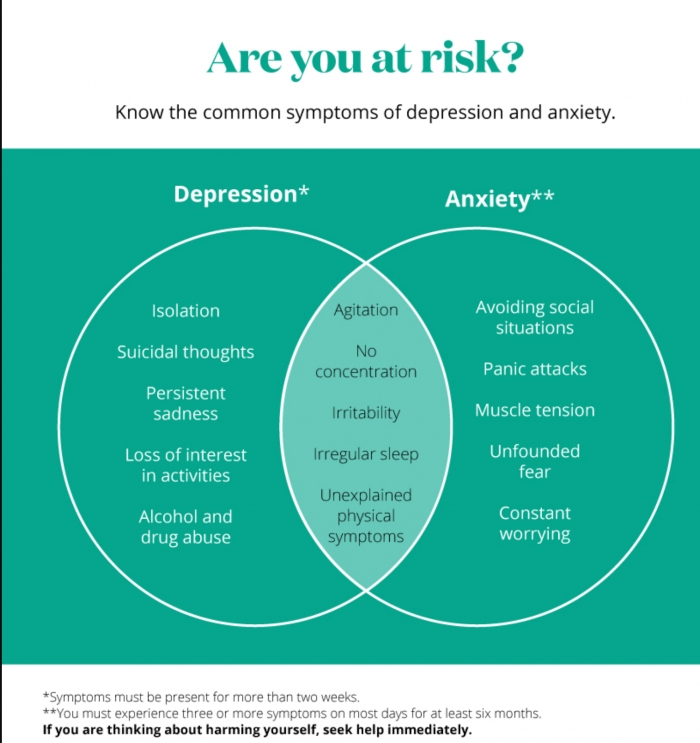
WHAT ARE THE SIGNS AND SYMPTOMS OF DEPRESSION?
 If you have been experiencing some of the following signs and symptoms most of the day, nearly every day, for at least two weeks, you may be suffering from depression:
If you have been experiencing some of the following signs and symptoms most of the day, nearly every day, for at least two weeks, you may be suffering from depression:
• Persistent sad, anxious, or “empty” mood
• Feelings of hopelessness, or pessimism
• Irritability
• Feelings of guilt, worthlessness, or helplessness
• Loss of interest or pleasure in hobbies and activities
• Decreased energy or fatigue
• Moving or talking more slowly
• Feeling restless or having trouble sitting still
• Difficulty concentrating, remembering, or making decisions
• Difficulty sleeping, early-morning awakening, or oversleeping
• Appetite and/or weight changes
• Thoughts of death or suicide, or suicide attempts
• Aches or pains, headaches, cramps, or digestive problems without a clear physical cause and/or that do not ease even with treatment
 Not everyone who is depressed experiences every symptom. Some people experience only a few symptoms while others may experience many. Several persistent symptoms in addition to low mood are required for a diagnosis of major depression, but people with only a few – but distressing – symptoms may benefit from treatment of their “subsyndromal” depression. The severity and frequency of symptoms and how long they last will vary depending on the individual and his or her particular illness. Symptoms may also vary depending on the stage of the illness.
Not everyone who is depressed experiences every symptom. Some people experience only a few symptoms while others may experience many. Several persistent symptoms in addition to low mood are required for a diagnosis of major depression, but people with only a few – but distressing – symptoms may benefit from treatment of their “subsyndromal” depression. The severity and frequency of symptoms and how long they last will vary depending on the individual and his or her particular illness. Symptoms may also vary depending on the stage of the illness.
WHAT ARE THE MAIN CAUSES OF DEPRESSION?
There are a number of factors that may increase the chance of depression, including the following:
• Abuse. Past physical, sexual, or emotional abuse can cause depression later in life.
• Certain medications. For example, some drugs used to treat high blood pressure, such as beta-blockers or reserpine, can increase your risk of depression.
• Conflict. Depression may result from personal conflicts or disputes with family members or friends.
• Death or a loss. Sadness or grief from the death or loss of a loved one, though natural, can also increase the risk of depression.
• Genetics. A family history of depression may increase the risk. It’s thought that depression is passed genetically from one generation to the next. The exact way this happens, though, is not known.
• Major events. Even good events such as starting a new job, graduating, or getting married can lead to depression. So can moving, losing a job or income, getting divorced, or retiring.
• Other personal problems. Problems such as social isolation due to other mental illnesses or being cast out of a family or social group can lead to depression.
WHAT ARE RISK FACTORS FOR DEPRESSION?
Depression is one of the most common mental disorders in the U.S. Current research suggests that depression is caused by a combination of genetic, biological, environmental, and psychological factors.
Depression can happen at any age but often begins in adulthood. Depression is now recognized as occurring in children and adolescents, although it sometimes presents with more prominent irritability than low mood. Many chronic mood and anxiety disorders in adults begin as high levels of anxiety in children.
Depression, especially in midlife or older adults, can co-occur with other serious medical illnesses, such as diabetes, cancer, heart disease, and Parkinson’s disease. These conditions are often worse when depression is present. Sometimes medications taken for these physical illnesses may cause side effects that contribute to depression. A doctor experienced in treating these complicated illnesses can help work out the best treatment strategy.
Risk factors include:
• Personal or family history of depression
• Major life changes, trauma, or stress
• Certain physical illnesses and medications
Does Depression Often Occur With Grief?
Grief is a common response to loss. Losses that may lead to grief include the death or separation of a loved one, loss of a job, death or loss of a beloved pet, or any number of other changes in life, such as divorce, becoming an “empty nester,” or retirement. Anyone can experience grief and loss, but not everyone will experience depression. Each person is unique in how he or she copes with these feelings.
Is Depression Linked to Chronic Pain?
When pain lingers for weeks to months, it’s referred to as being “chronic.” Not only does chronic pain hurt, it also disturbs your sleep, your ability to exercise and be active, your relationships, and your productivity at work. Can you see how chronic pain may also leave you feeling sad, isolated, and depressed?
There is help for chronic pain and depression. A multifaceted program of Pain medicine, psychotherapy, support groups, and more can help you manage your pain, ease your depression, and get your life back on track.
Can Certain Drugs Cause Depression?
In certain people, drugs may lead to depression. For example, medications such as barbiturates, benzodiazepines, and beta-blockers have been associated with depression, especially in older people. Likewise, medications such as corticosteroids, opioids (codeine, morphine), and anticholinergics taken to relieve stomach cramping have been found to cause mania, which is a highly elated state associated with bipolar disorder.
What’s the Link Between Depression and Chronic Illness?
In some people, a chronic illness causes depression. A chronic illness is an illness that lasts for a very long time and usually cannot be cured completely. However, chronic illnesses can often be controlled through diet, exercise, lifestyle habits, and certain medications. Some examples of chronic illnesses that may cause depression are diabetes, heart disease, arthritis, kidney disease, HIV/AIDS, lupus, and multiple sclerosis (MS). Hypothyroidism may also lead to depressed feelings. Researchers believe that treating depression may also help co-existing illness improve.
Treatment and Therapies?
Depression, even the most severe cases, can be treated. The earlier that treatment can begin, the more effective it is. Depression is usually treated with medications, psychotherapy, or a combination of the two. If these treatments do not reduce symptoms, electroconvulsive therapy (ECT) and other brain stimulation therapies may be options to explore.
AT OUR CENTER, YOUR LIFE CHANGE, WE OFFER ONE FORM OF THERAPY REFERRED AS INDIVIDUAL THERAPY
INDIVIDUAL THERAPY.
Individual therapy is a shared process between a therapist and a person in treatment. The therapist seeks to assist the individual in managing issues that are challenging to deal with alone. This model of therapy is also known as psycho-social therapy, talk therapy, psychotherapy, and cognitive-behavioral counseling.
Individual Therapy: Our Goals
Many of life’s challenges can be extremely difficult to manage. The pressures that are placed on us can be overwhelming, especially when we face them alone. With this thought in mind, there are two key goals that we seek to achieve while assisting a patient during our therapy sessions.
Our first goal is to assist the individual in overcoming obstacles that interfere with the individuals’ mental-wellness. Our second goal is to stimulate change in the thinking patterns of the individual showing them how to move their thoughts towards improving their conditions.
The focus of Individual Therapy efforts center on areas of individuals’ lives that they have a concern. These areas commonly involve conditions that are causing a great deal of distress in the individual’s life. Distress in this sense generally means:
People seek therapy for reasons such as coping with significant life challenges, dealing with trauma, depression, and anxiety are the most common ones.
Benefits of Individual Therapy?
There’s a wide range of rewards that a person may benefit as a result of Individual Therapy. Some examples of these advantages are:
• Increased compassion and self-esteem
• The acquisition of skills to aid in handling stressful situations
• Comprehension of how to make healthy decisions can lead to self-growth.
• Development of the proclivity for establishing and following through on plans of action.
Aside from the benefits listed above, many people find that they enjoy the therapeutic process of becoming more self-aware. It helps to understand themselves and others better. It also helps them set personal goals and work toward desired change.
• You are experiencing bodily sensations such as pain or fatigue,
• You are often unhappy,
• You feel overwhelmed and hopeless about issues in your life,
• You cannot focus on work or school,
• You are experiencing addiction,
• You feel like hurting yourself or someone else.
We’re Here to Help. If you find it difficult to deal with an issue that is causing distress or interfering with your day-to-day life, counseling may be a good solution.
Beyond Treatment: Things You Can Do?
Here are other tips that may help you or a loved one during treatment for depression:
• Try to be active and exercise.
• Set realistic goals for yourself.
• Try to spend time with other people and confide in a trusted friend or relative.
• Try not to isolate yourself, and let others help you.
• Expect your mood to improve gradually, not immediately.
• Postpone important decisions, such as getting married or divorced, or changing jobs until you feel better. Discuss decisions with others who know you well and have a more objective view of your situation.
• Continue to educate yourself about depression.
The information in this document does not replace a medical consultation. It is for personal guidance use only. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of the disease.